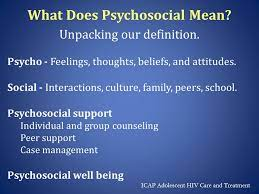
Get an assessment assistance on What is the definition of psychosocial care?
Recognized Crisis Reactions include: withdrawing from social interaction; fighting; fleeing; and freezing
Apathy and disassociation
Trembling and swaying
No symptoms at all; no symptoms for the first few of days; followed by the emergence and development of symptoms
Acute symptoms that go away after a few days, acute symptoms that worsen over time, and persistent low-level symptoms.
Increased substance dependency and somatic symptoms
Disturbances in sleep
Inability to perform
Intervention by a Professional or Paraprofessional Etc.
After a crisis, the issue of whether professionals should step in or if paraprofessionals like friends, family, and laypeople may help the victim heal emerges.
According to studies on crisis recovery, we must monitor the progress of individuals after a disaster. Professional sense urges us not to act in cases when a patient has no symptoms or whose symptoms are settling and stabilizing with time. It is advisable to leave them in the care of paraprofessionals or naturalistic rehabilitation.
Naturalistic rehabilitation includes taking time away from the crisis event, connecting with loved ones, being in comfortable and secure circumstances, going to locations that make you feel refreshed, spending time with pets, being close to the ocean or a forest, speaking with a church member or pastor, and talking to other survivors about your experience. Monitoring Are drugs necessary, and only if symptoms do not improve after contacting a professional? Some survivors may need medication if their symptoms are still impairing their ability to operate normally. The optimal course of medication should be brief and under strict physician supervision. Dependency issues must be assessed and carefully addressed. Medication side effects must also be carefully monitored, especially increased social withdrawal and impulsivity, including self-harm and suicidal ideation. Professional intervention may be necessary for those whose symptoms are getting worse over time (for more than a week or more). A referral to a doctor may be necessary, as well as crisis and trauma counseling.
Richard K. James Crisis Intervention Model
Gilliland and James (1998) a 6-step process
- Determine the issues or threats
- Ensure safety; 3. Offer assistance
- Consider substitutes
- Make plans for reestablishing balance.
- Convince yourself to take action.
Following their stage model for 20 years “We no longer believe that a stage or purely step model captures the way crisis intervention works, and here’s why,” write James and Gilliland in 2013. Since crisis is sometimes anything but linear, it has been difficult for us to educate students like you about crisis intervention. Crisis intervention often exemplifies chaos theory, with all of its starts, pauses, do-overs, and U-turns, according to page 51.
Crisis workers’ range of action includes: o Being directive when the client is immobile; o Being collaborative when the client is only partly mobile.
o The worker is nondirective while the customer is on the go.
Robert’s Crisis Intervention Model
The abbreviation for Roberts’ (2005) ACT model is:
Evaluation of the current issue, including mental and other urgent medical requirements, as well as trauma evaluation
Linking customers with assistance resources
Post-traumatic stress disorders and traumatic responses
Seven-step model - Evaluate the situation 2. Build rapport
- Identify the biggest issues
- Handle emotions
- Come up with and research alternatives
- Create plans
- Include a follow-up.
The equilibrium model is really a model of equilibrium and disequilibrium.
People who are experiencing a crisis are in a condition of psychological or emotional unease in which their typical coping strategies and means of problem-solving don’t suffice. The equilibrium model’s objective is to assist individuals in regaining their pre-crisis equilibrium (Caplan, 1961).
Cognition Model
The cognitive model of crisis intervention is predicated on the idea that crises are not caused by the events themselves or by the facts surrounding the events or circumstances, but rather by incorrect thinking about those events or situations (Ellis, 1962). This concept seeks to modify people’s perspectives and ideas regarding crisis circumstances or occurrences by assisting them in becoming aware of them. The fundamental tenet of the cognitive model is that people can change their thinking and take control of life crises, particularly by identifying and contesting the irrational and self-defeating aspects of their cognitions while retaining and emphasizing the rational and self-enhancing aspects.
The psychosocial transition concept is based on the idea that individuals are a combination of their genes and the knowledge they have gleaned from their unique social surroundings. Crises may be caused by issues that are internal or external (psychological, social, or environmental). The aim of crisis intervention is to work with clients to identify the internal and external factors leading to the crisis and then support them in making practical changes to their present attitudes, behaviors, and resource utilization. In order to regain autonomous (non-crisis) control over their life, clients may need to include suitable internal coping strategies, social supports, and environmental resources.
Collins and Collins (2005) created a developmental-ecological model of crisis intervention that takes into account the individual’s surroundings as well as their developmental stages and problems. According to this paradigm, the crisis worker must evaluate the client, the surroundings, and their interactions before taking into account the client’s current developmental stage.
Any situational crisis must always be taken into account in connection to the developmental stage the person is at, and the severity of the crisis may depend on how successfully the tasks impacted by the crisis have been stage-mastered.
Myer and Moore (2006) provide a method for calculating the effect of a crisis on a person or system called the Contextual-Ecological Model. The equation may be summed up as a function of closeness to the event, response to the event, relationship to the event, and the amount of change the event created, which is then divided by the passage of time. Understanding that no one element of this formula may be taken into account independently is crucial.
Mental Health First Aid on What is the definition of psychosocial care?
According to the National Institute of Mental Health (2002), psychological first aid include making sure the client is secure, minimizing stress-related symptoms, allowing for relaxation and physical recovery, and connecting clients with vital services and social support networks. In her description of crisis work after the Granville train catastrophe, Raphael (1977) adopted the phrase psychological first aid. She discussed a range of initiatives that gave survivors compassionate care, empathetic responses, specific information and help, and the chance to reconnect with their social support networks.
Paying attention to Maslow’s hierarchy and putting survival requirements first are essential components of psychological first aid.
Tyhurst first used the phrase “psychological first aid” in 1951.
An evidence-based, modular method for helping individuals in the early aftermath of catastrophe and terrorism to minimize initial distress and to nurture short- and long-term adaptive functioning was more recently refined into a particular intervention (NC-PTSD).
“Basic, non-intrusive pragmatic care” is defined by the Sphere Project (2004) as “basic, non-forcing talk, needs assessment, and ensuring that basic needs are met, encouraging but not forcing company from significant others, and protecting from further harm.”
PFA’s constituent parts (North Atlantic Treaty Organization, 2009)
Comfort and solace, safety from additional danger and distress, immediate medical attention, encouragement of goal-oriented and purposeful behavior, assistance in reuniting people with loved ones, opportunity for voluntary sharing of experiences, connecting survivors with resources of support, facilitation of a sense of control, and triage of those in need of additional assistance.
The Inter-agency Standing Committee’s 2007 report on PFA’s components
identifying and addressing basic practical needs and concerns o discouraging negative coping mechanisms o encouraging regular daily routines and positive coping o encouraging, but not pressuring, company from family or friends o providing the opportunity to return for additional support o providing referrals to local support or clinicians
PFA Provision o It is critical that the PFA tenets can be swiftly taught to both volunteers and professionals, including those with and without prior experience in mental health. Some types of psychological support, for example, don’t need for specialized knowledge and may be easily taught to workers without such training (IASC).
- ………Get more on What is the definition of psychosocial care?
